Numerous assessment tools exist to assist in the measurement and monitoring of symptoms and their impact.[1] These tools should be used appropriately and not as a substitute for a comprehensive, holistic assessment. Tools should be reliable, valid, evidence-based and not adapted to meet local needs unless they are revalidated within that population or setting.[2]
Using validated assessment tools promotes:[3-4]
- A level of security and understanding for the person, their family and carers that:
- the multidimensional aspects of symptoms are being thoroughly considered on a regular basis
- care is consistent and coordinated
- A systematic approach to assessing the multidimensional nature of symptoms
- A cohesive language of reporting between health professionals, which provides an accurate and concise picture of the person’s symptoms and comfort level.
Assessment tools can be designed to:
- Assess multiple symptoms eg, the Symptom Assessment Scale (SAS).[4] These tools are useful in routine practice for screening to identify people experiencing symptoms.
- Identify specific needs within a domain in order to provide relevant care/services eg, The FICA Spiritual History Tool.[5]
- Guide the assessment of a specific symptom eg, the brief pain inventory.[6] These tools enable a more comprehensive assessment to identify causes and effects of individual symptoms.
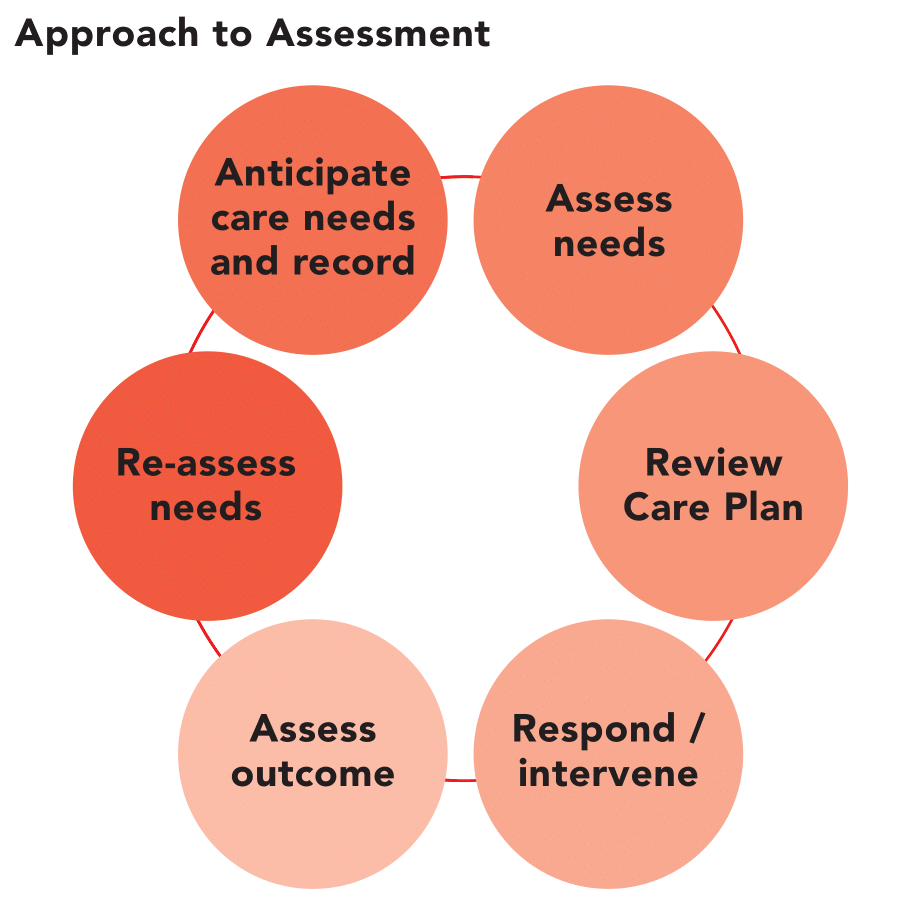
Assessment and reassessment are core elements of the person’s care as outlined in the following figure:[1]
Palliative assessment tool examples
The Palliative Care Outcomes Collaboration (PCOC) is a national program that facilitates the use of standardised clinical assessment tools to measure and benchmark outcomes in palliative care. Palliative care assessment tools commonly used throughout Australia are summarised in the following table:[4]
| Assessment Tool | Purpose |
| Palliative Care Problem Severity Score (PCPSS) | Clinician rated score of palliative care concerns that provides a summary measure of concerns in four domains: pain, other symptoms, psychological / spiritual and family / carer.[10] |
| Symptom Assessment Scale (SAS) | The SAS is rated by the person with a life-limiting illness, rather than a clinician. It assesses the degree of distress relating to seven common symptoms and identifies the person’s priorities relating to specific symptoms.[7, 11] |
| Functional Assessment in Palliative Care (RUG-ADL) | This four-item scale measures motor function with activities of daily living: bed mobility, toileting, transfer and eating. Assessment is based on what the person does, not what they are capable of doing. It provides information on functional status, the assistance the person requires to carry out these activities and the resources needed for their care.[12] |
| Australia-modified Karnofsky Performance Status (AKPS) | The AKPS is a single score between 10 and 100 assigned by a clinician based on observations of a person’s ability to perform common tasks relating to activity, work and self-care.[12] |
The Palliative Aged Care Outcomes Program (PACOP) aims to significantly improve the outcomes of all Australians in aged care homes with a particular focus on those who are approaching the end of their life. PACOP supports aged care facilities to embed the use of standardised outcomes assessments and tools, and to use the information gathered to respond in a timely way.
Thinking Points
- What can the Symptom Assessment Scale (SAS) and Palliative Care Problem Severity Score (PCPSS) tell us about Herbert’s breathlessness?
- Comment on whether these tools assesses the multiple dimensions of the symptom
- Comment on how these tools assesses the individual’s experience of the symptom
- What advantages and limitations would these assessment tools have in practice? Provide reasons for your answer.
- What assessment tools can you use to assess a person’s psychological wellbeing?
References
- Therapeutic Guidelines. 2023. Principles of symptom management. Melbourne.
- McIlfatrick, S. and F. Hasson. 2014. Evaluating an holistic assessment tool for palliative care practice. J Clin Nurs. 23(7-8): p. 1064-75.
- CareSearch. 2022. Assessment in Ongoing Care.
- Palliative Care Outcomes Collaboration. 2024. PCOC Assessment Tools.
- Puchalski, C. 1999. FICA Spiritual Assessment Tool.
- Philip, J., et al. 1998. Concurrent validity of the modified Edmonton Symptom Assessment System with the Rotterdam Symptom Checklist and the Brief Pain Inventory. Supportive Care in Cancer. 6(6): p. 539-541.